Please note, this page contains supplementary information and is not a component of the eLearning course.
Opioid tapering
This section offers a step-by-step guide to managing the opioid reduction, where this has been agreed with the patient.
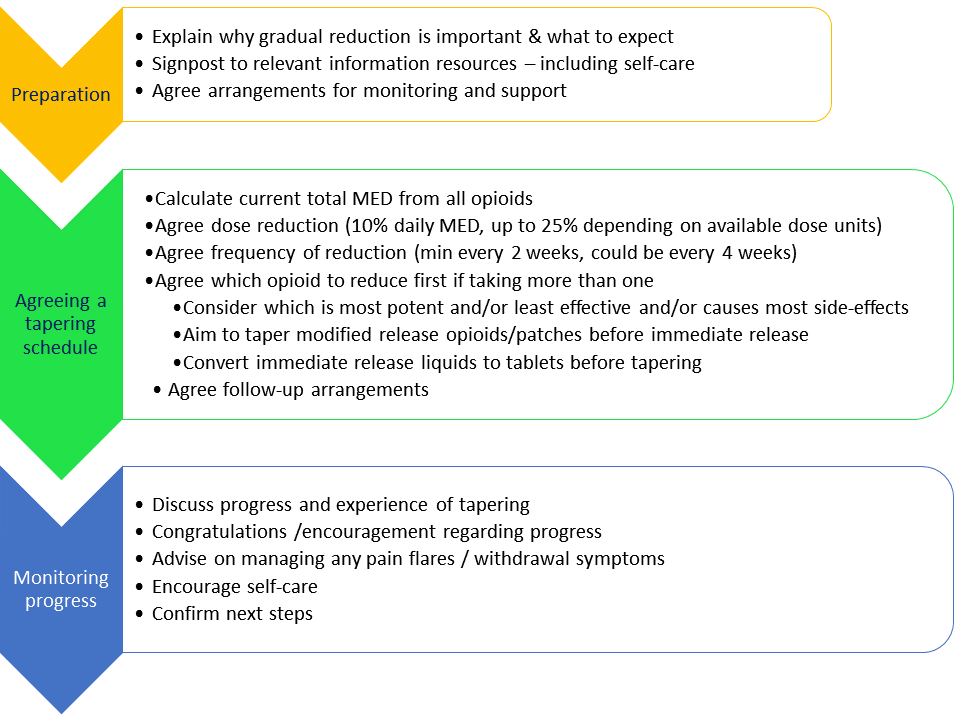
Preparing the patient for tapering
- Make sure the patient knows that opioids should be tapered gradually and not stopped suddenly and that the reduction will take time, often months not weeks, especially if they are on high doses
- Explain what to expect including:
- Whilst it is unlikely that pain will increase longer-term, some patients experience tiredness, restlessness, and/or an increase in their usual pain following opioid dose reduction
- Only a few people report withdrawal symptoms (see box below) following gradual tapering, although patients may fear this if they have stopped or reduced opioids abruptly in the past
Withdrawal Symptoms
Patients experience withdrawals differently and may experience none, some, or all of the following symptoms:
- Sweating
- Yawning
- Tremor
- Abdominal cramps
- Diarrhoea
- Restlessness
- Irritability
- Anxiety
- Runny nose/eyes
- Bone or joint aches, which may be confused with perceived worsening of the original pain
- Reassure that withdrawal symptoms are temporary and any increase in their usual pain is unlikely to persist long-term. Most people do not experience worse pain following opioid reduction and many notice an overall improvement because they are having fewer side effects
- Encourage the patient to reflect on their previous experience of pain symptoms fluctuating, with ‘good and ‘bad’ days even when opioids remained stable or were increasing and explain that this variation is likely to continue
- Discuss self-management (self-care) strategies (see training manual section 3.2, Supporting self-care strategies)
- Signpost to relevant information resources about opioid tapering (see training manual section 2.6, Talking about opioids and 4.5, Patient information resources)
- Reassure them about how you will monitor and support them during the taper. Including arrangements for follow-up appointments and ‘as required’ contact between appointments (see training manual section 3.5, Next steps)
Creating a tapering schedule with the patient
- Agree whether the goal is stopping or tapering to lowest effective dose (with the option to consider further reduction then)
- Calculate total oral morphine equivalence of all current opioids by any route
- Check with the patient what they are actually taking, don’t assume the prescribed dose is being taken
- Use the opioid equianalgesic calculator developed by the Faculty of Pain Medicine, Australian and New Zealand College of Anaesthetists (FPM ANZCA), to calculate the total morphine equivalent daily dose (MED). The calculator is available here and can also be downloaded as a smart phone application from the Apple App Store or Google Play Store
- Avoid switching to a different opioid in order to taper, instead reduce the dose of their currently prescribed opioid(s)
- Aim to taper the dose by around 10% of the original dose two weekly or monthly
- The exact % reduction will depend on the dose units available
- If the patient is particularly anxious, starting with a smaller dose decrease (e.g. 5% or even less) and reducing monthly, may help build confidence
- Avoid reducing more frequently than every 2 weeks
- When considering frequency of reductions, consider your capacity for follow up and review, taking into account any periods of leave
- Remember that the dose reduction becomes a larger proportion of the dose as the dose reduces. Consider smaller dose reductions as the dose becomes lower, if the patient starts to run into difficulty
- If a patient is taking more than one opioid, reduce one at a time. Ideally start with the most potent
- If a patient is taking oral modified release (MR) opioids (including patches) as well as immediate release (IR), taper the MR / patch first. If they are taking IR liquid, switch to tablets to more easily monitor the amount used
- Limit number of doses of IR per day and counsel patient not to increase dose of IR to compensate
- Ensure that prescriptions are not issued early
- When reducing a fentanyl patch, bear in mind that the lowest dose patch available is 12 mcg/hour (MED 36mg/day). Dependent on how well the patient has tolerated previous reductions, for the final tapering step, you may wish to consider advising that they cut a 12 mcg/ hour matrix patch in half. Please note this only acceptable if they are prescribed a matrix patch
- Agree the frequency of monitoring and how this will be done with the patient. For example: arranging monthly follow-up appointments, with a telephone call after the first 2 weeks
Monitoring progress
- Check whether the patient has been able to adhere to the tapering plan and whether there has been any change in usual pain/ function and whether they have experienced any withdrawal symptoms
- Offer advice on managing pain flares and / or withdrawal symptoms if needed (see below)
- Offer encouragement for their progress so far and remind them of their reasons for tapering
- Re-evaluate whether a patient is ready to take the next step in their tapering plan and what support is required
Dealing with increased pain and/or withdrawal symptoms
- Tapering may be paused to allow time to overcome symptoms of withdrawal or worse pain before the next dose reduction
- However, tapering should not be reversed except in exceptional circumstances
- Do not be tempted to treat withdrawal symptoms with more opioids or benzodiazepines
- Reassure your patient that persistent pain varies over time, as it most likely did prior to them starting the opioid taper, and any increase following dose reduction is likely to be temporary
- Remind them why they decided to make changes to their opioid medicines in the first place, and the potential benefits of tapering for them
- Encourage patients:
- to be kind to themselves,
- to make time to do the things they find enjoyable and/or comforting and soothing,
- to consider taking some gentle exercise,
- to get support from friends or family (see training manual section 3.2.4, Set-back planning)
- Signpost to videos of patients who have successfully reduced opioids that they may find inspiring (see training manual section 4.5, Patient information resources).
We recommend using the ANZCA Opioid Calculator to calculate daily Morphine Equivalent Dose (MED).
You can download the Opioid Calculator App for mobile devices from App Store and Google Play and a desktop version is also available
Please note that opioid conversion factors are an approximate guide only because comprehensive data are lacking and there is significant inter-individual variation. You will find slightly different values from difference sources. The ANZCA app does not include dihydrocodeine and you can use the conversion factor for codeine instead.
CDC Guideline for Prescribing Opioids for Chronic Pain (US)